What Is Gestational Diabetes?
Gestational diabetes is a type of diabetes that develops during pregnancy when your body can’t make enough insulin to regulate blood sugar effectively. Unlike type 1 or type 2 diabetes, it typically resolves after childbirth, but it still requires careful management during pregnancy to protect your health and your baby’s development.
Who’s at Risk?
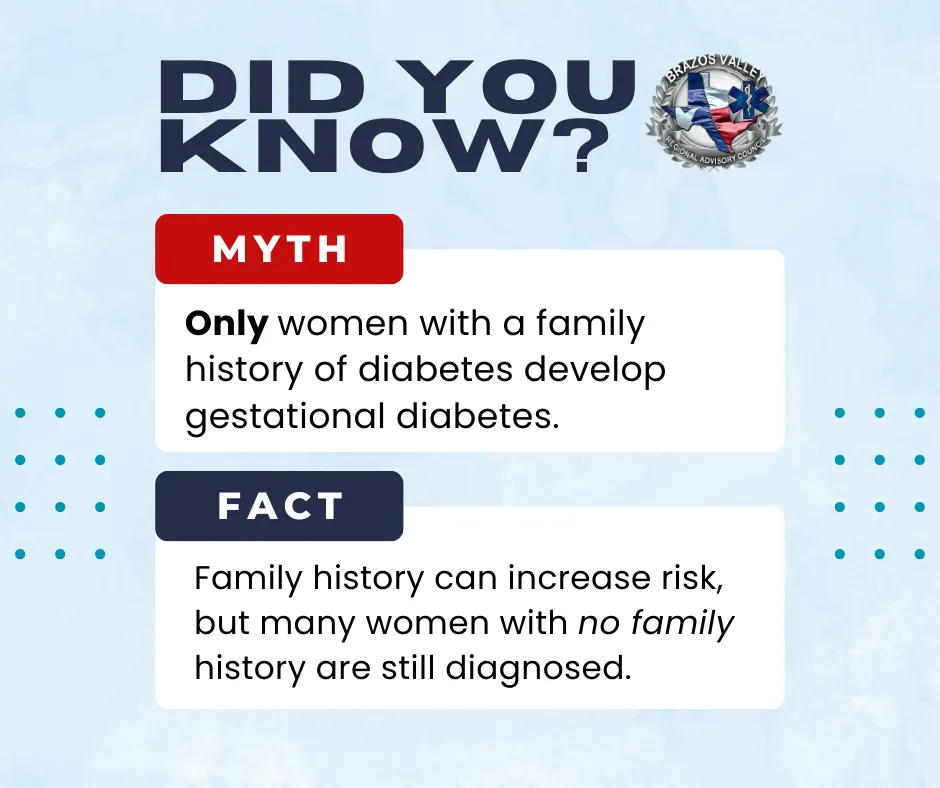
While any pregnant woman can develop gestational diabetes, certain factors increase the risk, including:
- Being over age 25
- Having a family history of type 2 diabetes
- Being overweight before pregnancy
- Previous history of gestational diabetes
- Having given birth to a baby weighing over 9 pounds
- Belonging to certain ethnic groups with higher risk rates
Even if you don’t have these risk factors, gestational diabetes can occur, which is why routine prenatal screenings are so important.
How Is It Diagnosed?
Most providers screen for gestational diabetes between 24 and 28 weeks of pregnancy with an oral glucose tolerance test. If your blood sugar levels are above the recommended range, your provider will work with you on a plan to manage them through nutrition, activity, and possibly medication.
Why Nutrition Matters
What you eat has a direct impact on your blood sugar levels. The goal is to choose foods that provide steady energy without causing spikes. This isn’t about “eating for two” in the sense of doubling portions; it’s about eating nutrient-rich, balanced meals that support both you and your baby.
Nutrition Tips for a Healthy Pregnancy with Gestational Diabetes
- Focus on Complex Carbs
Choose whole grains like oatmeal, brown rice, whole wheat bread, and quinoa. Pair carbs with protein or healthy fats to slow digestion and keep blood sugar steady. - Load Up on Non-Starchy Vegetables
Spinach, broccoli, bell peppers, zucchini, and leafy greens are low in carbs and high in vitamins, minerals, and fiber. - Choose Lean Proteins
Incorporate poultry, fish (low-mercury varieties), eggs, beans, and lentils into your meals to support healthy growth and satiety. - Watch Your Fruit Portions
Fruit is healthy but contains natural sugars. Opt for berries, apples, and pears, and pair them with protein or fat to reduce blood sugar spikes. - Limit Sugary Drinks & Snacks
Skip sodas, sweet teas, candy, and pastries. If you want a sweet treat, choose naturally sweet foods like a small serving of fresh fruit. - Eat Regularly
Skipping meals can cause blood sugar dips and spikes. Aim for three balanced meals and two to three healthy snacks each day. - Stay Hydrated
Water is the best choice. Adequate hydration supports your metabolism and overall pregnancy health.

What Happens After Delivery?
In most cases, gestational diabetes resolves after birth. However, women who have had it are at a higher risk of developing type 2 diabetes later in life. Maintaining a healthy lifestyle postpartum, including regular physical activity and balanced eating, can help lower this risk.
Final Thoughts
Gestational diabetes doesn't have to overshadow your pregnancy. With the right knowledge, nutrition, and care plan, you can protect your health and support your baby's development.
If you have questions or need local support, talk to your healthcare provider. Early diagnosis and consistent management are key to a healthy pregnancy and delivery.
Brazos Valley Regional Advisory Council (BVRAC) is committed to promoting maternal and infant health through education and community resources. If you are pregnant or planning a pregnancy, speak with your healthcare provider about your risk for high blood pressure and how to manage it.